How to Get Your Gun Rights Back for Mental Illness
The COVID-19 pandemic and the resulting economic recession have negatively affected many people's mental health and created new barriers for people already suffering from mental illness and substance use disorders. During the pandemic, about 4 in 10 adults in the U.S. have reported symptoms of anxiety or depressive disorder, a share that has been largely consistent, up from one in ten adults who reported these symptoms from January to June 2019 (Figure 1). A KFF Health Tracking Poll from July 2020 also found that many adults are reporting specific negative impacts on their mental health and well-being, such as difficulty sleeping (36%) or eating (32%), increases in alcohol consumption or substance use (12%), and worsening chronic conditions (12%), due to worry and stress over the coronavirus. As the pandemic wears on, ongoing and necessary public health measures expose many people to experiencing situations linked to poor mental health outcomes, such as isolation and job loss.
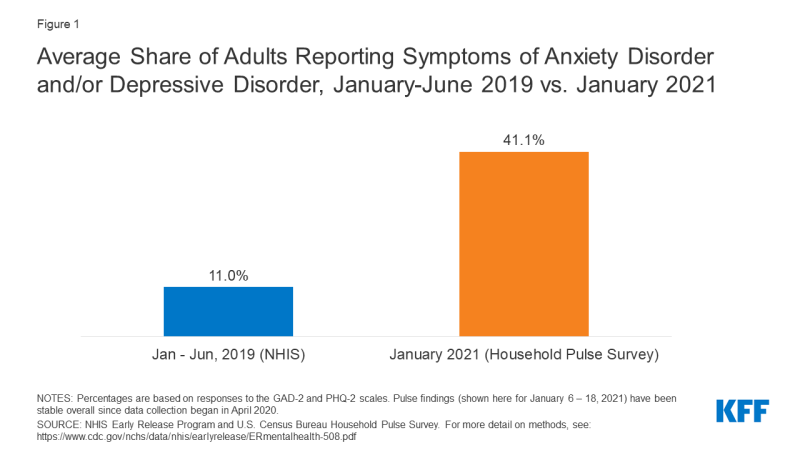
Figure 1: Average Share of Adults Reporting Symptoms of Anxiety Disorder and/or Depressive Disorder, January-June 2019 vs. January 2021
This brief explores mental health and substance use during, and prior to, the COVID-19 pandemic. It focuses on populations that were particularly at risk for experiencing negative mental health or substance abuse consequences during the pandemic, including young adults, people experiencing job loss, parents and children, communities of color, and essential workers. We draw on KFF analysis of data from the Census Bureau's Household Pulse Survey (an ongoing survey created to capture data on health and economic impacts of the pandemic), KFF Health Tracking Poll data, and data on mental health prior to the COVID-19 pandemic. Key takeaways include:
- Young adults have experienced a number of pandemic-related consequences, such as closures of universities and loss of income, that may contribute to poor mental health. During the pandemic, a larger than average share of young adults (ages 18-24) report symptoms of anxiety and/or depressive disorder (56%). Compared to all adults, young adults are more likely to report substance use (25% vs. 13%) and suicidal thoughts (26% vs. 11%). Prior to the pandemic, young adults were already at high risk of poor mental health and substance use disorder, though many did not receive treatment.
- Research from prior economic downturns shows that job loss is associated with increased depression, anxiety, distress, and low self-esteem and may lead to higher rates of substance use disorder and suicide. During the pandemic, adults in households with job loss or lower incomes report higher rates of symptoms of mental illness than those without job or income loss (53% vs. 32%).
- Research during the pandemic points to concerns around poor mental health and well-being for children and their parents, particularly mothers, as many are experiencing challenges with school closures and lack of childcare. Women with children are more likely to report symptoms of anxiety and/or depressive disorder than men with children (49% vs. 40%). In general, both prior to, and during, the pandemic, women have reported higher rates of anxiety and depression compared to men.
- The pandemic has disproportionately affected the health of communities of color. Non-Hispanic Black adults (48%) and Hispanic or Latino adults (46%) are more likely to report symptoms of anxiety and/or depressive disorder than Non-Hispanic White adults (41%). Historically, these communities of color have faced challenges accessing mental health care.
- Many essential workers continue to face a number of challenges, including greater risk of contracting the coronavirus than other workers. Compared to nonessential workers, essential workers are more likely to report symptoms of anxiety or depressive disorder (42% vs. 30%), starting or increasing substance use (25% vs. 11%), and suicidal thoughts (22% vs. 8%) during the pandemic.
Both those newly experiencing mental health or substance abuse disorders and those already diagnosed before the pandemic may require mental health and substance use services but could face additional barriers because of the pandemic.
Prevalence of Mental Illness and Substance Use Disorder During the Pandemic
During the COVID-19 pandemic, concerns about mental health and substance use have grown, including concerns about suicidal ideation. In January 2021, 41% of adults reported symptoms of anxiety and/or depressive disorder (Figure 2), a share that has been largely stable since spring 2020. In a survey from June 2020, 13% of adults reported new or increased substance use due to coronavirus-related stress, and 11% of adults reported thoughts of suicide in the past 30 days. Suicide rates have long been on the rise and may worsen due to the pandemic. Early 2020 data show that drug overdose deaths were particularly pronounced from March to May 2020, coinciding with the start of pandemic-related lockdowns.
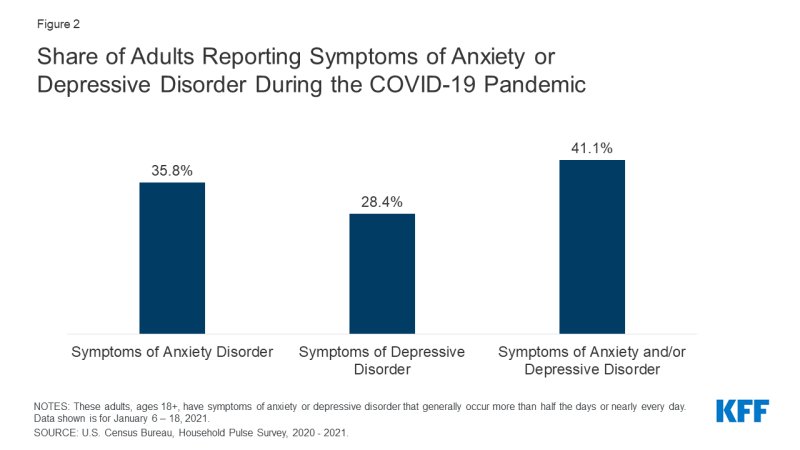
Figure 2: Share of Adults Reporting Symptoms of Anxiety or Depressive Disorder During the COVID-19 Pandemic
As was the case prior to the pandemic, adults in poor general health (which may reflect both physical and mental health) continue to report higher rates of anxiety and/or depression than adults in good general health.1 , 2 For people with chronic illness in particular, the already high likelihood of having a concurrent mental health disorder may be exacerbated by their vulnerability to severe illness from COVID-19. Recently, a study also found that 18% of individuals (including people with and without a past psychiatric diagnosis) who received a COVID-19 diagnosis were later diagnosed with a mental health disorder, such as anxiety or mood disorders. Older adults are also more vulnerable to severe illness from coronavirus and have experienced increased levels of anxiety and depression during the pandemic.
Mental distress during the pandemic is occurring against a backdrop of high rates of mental illness and substance use that existed prior to the current crisis. Prior to the pandemic, one in ten adults reported symptoms of anxiety and/or depressive disorder. Nearly one in five U.S. adults (47 million) reported having any mental illness. In 2018, over 48,000 Americans died by suicide,3 and on average across 2017 and 2018, nearly eleven million adults reported having serious thoughts of suicide in the past year. Additionally, deaths due to drug overdose were four times higher in 2018 than in 1999, driven by the opioid crisis.
There are a variety of ways the pandemic has likely affected mental health, particularly with widespread social isolation resulting from necessary safety measures. A broad body of research links social isolation and loneliness to both poor mental and physical health. The widespread experience of loneliness became a public health concern even before the pandemic, given its association with reduced lifespan and greater risk of both mental and physical illnesses. A KFF Health Tracking Poll conducted in late March 2020, shortly after many stay-at-home orders were issued, found those sheltering-in-place were more likely to report negative mental health effects resulting from worry or stress related to coronavirus compared to those not sheltering-in-place.
Some prior epidemics have induced general stress and led to new mental health and substance use issues. As the COVID-19 pandemic continues, different populations are at increased risk to experience poor mental health and may face challenges accessing needed care.
Young Adults
Throughout the pandemic, anxiety, depression, sleep disruptions, and thoughts of suicide have increased for many young adults. They have also experienced a number of pandemic-related consequences – such as closures of universities, transitioning to remote work, and loss of income or employment – that may contribute to poor mental health. KFF analysis of the Household Pulse Survey finds that throughout the pandemic, a large share of young adults (ages 18-24) have reported symptoms of anxiety and/or depressive disorder – 56% as of December 2020 – compared to older adults (Figure 3).
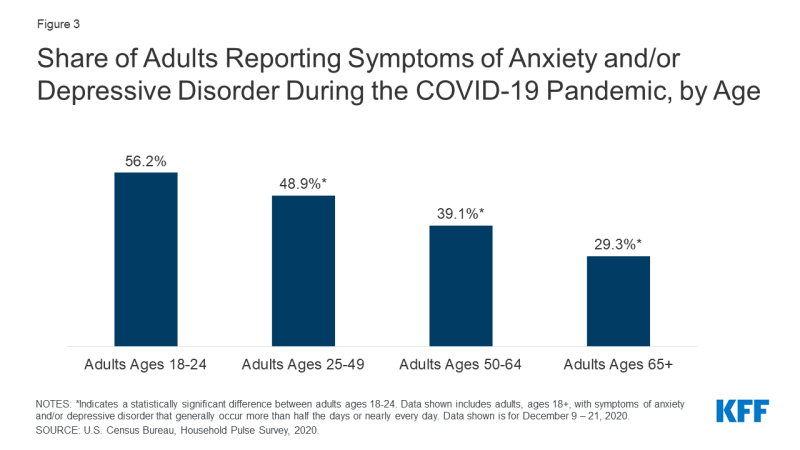
Figure 3: Share of Adults Reporting Symptoms of Anxiety and/or Depressive Disorder During the COVID-19 Pandemic, by Age
An earlier survey from June 2020 showed similar findings for young adults relative to all adults. The survey also found that substance use and suicidal ideation are particularly pronounced for young adults, with 25% reporting they started or increased substance use during the pandemic (compared to 13% of all adults), and 26% reporting serious thoughts of suicide (compared to 11% of all adults). Prior to the coronavirus outbreak, young adults were already at high risk of poor mental health and substance use disorder, yet many did not receive treatment.
Adults Experiencing Job Loss or Income Insecurity
Throughout the pandemic, many people across the country have experienced job or income loss, which has generally affected their mental health. Adults experiencing household job loss during the pandemic have consistently reported higher rates of symptoms of anxiety and/or depressive disorder compared to adults not experiencing household job loss (53% vs. 32%, respectively; Figure 4). Similarly, findings from the December KFF Health Tracking Poll show that households experiencing income or job loss are significantly more likely to report that worry or stress over the coronavirus outbreak has negatively impacted their mental health.
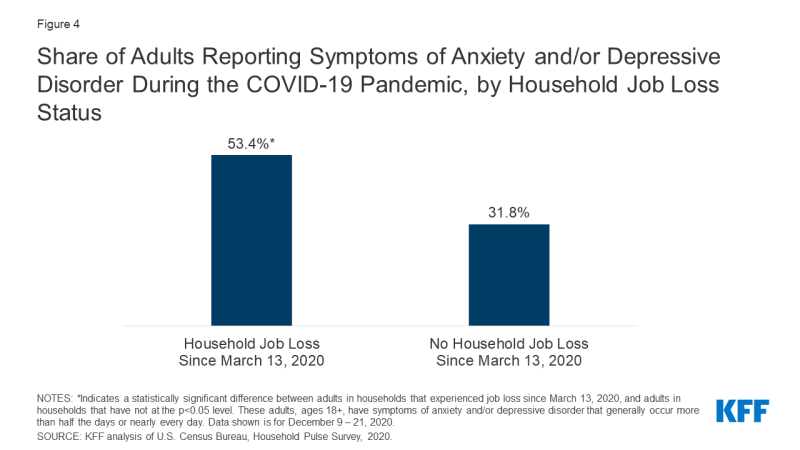
Figure 4: Share of Adults Reporting Symptoms of Anxiety and/or Depressive Disorder During the COVID-19 Pandemic, by Household Job Loss Status
In addition to increased anxiety and depression, job loss may lead to other adverse mental health outcomes, such as substance use disorder. During the previous recession, the high unemployment rate was also associated with increases in suicides. A KFF Health Tracking Poll conducted in mid-July 2020 found that, compared to households with no lost income or employment, a higher share of households experiencing income or job loss reported that pandemic-related worry or stress caused them to experience at least one adverse effect on their mental health and well-being, such as difficulty sleeping or eating, increases in alcohol consumption or substance use, and worsening chronic conditions (46% vs. 59%, respectively).4
KFF Health Tracking Polls conducted during the pandemic have also found that people with lower incomes are generally more likely to report major negative mental health impacts from worry or stress over the coronavirus. In December 2020, 35% of those earning less than $40,000 reported experiencing a major negative mental health impact, compared to 21% of those with incomes between $40,000 to $89,999 and 17% of those making $90,000 or more (Figure 5).
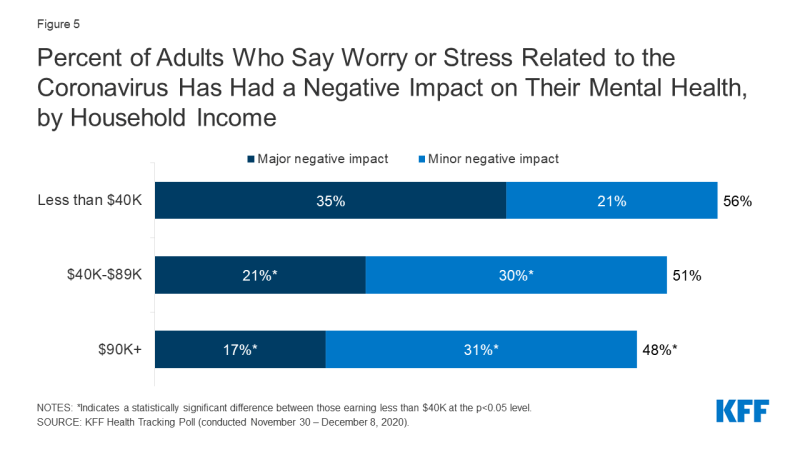
Figure 5: Percent of Adults Who Say Worry or Stress Related to the Coronavirus Has Had a Negative Impact on Their Mental Health, by Household Income
Parents and Children
To help slow the spread of coronavirus, many schools and childcare centers across the U.S. have closed and transitioned to virtual instruction for at least some time. With these closures, children and their parents are experiencing ongoing disruption and changes to their daily routines. Research during the pandemic highlights concerns around poor mental health and well-being for children and their parents. For example, many parents with school-aged children are now more concerned about their children's emotional well-being than prior to the pandemic. Both parents and their children have experienced worsening mental health since the start of the pandemic, and women with children are more likely than their male counterparts to report worsening mental health.
Throughout the pandemic, we find that adults in households with children under the age of 18, compared to adults in households without, are slightly more likely to report symptoms of anxiety and/or depressive disorder (45% vs. 41%, respectively, as of December 2020).5 Specifically, among households with children under the age of 18, women have been more likely than men to report symptoms of anxiety and/or depressive disorder throughout the pandemic (as of December 2020, 49% vs. 40%, respectively; Figure 6). Similarly, KFF Health Tracking Polls conducted during the pandemic have generally found that among parents, women are more likely than men to report negative mental health impacts.6
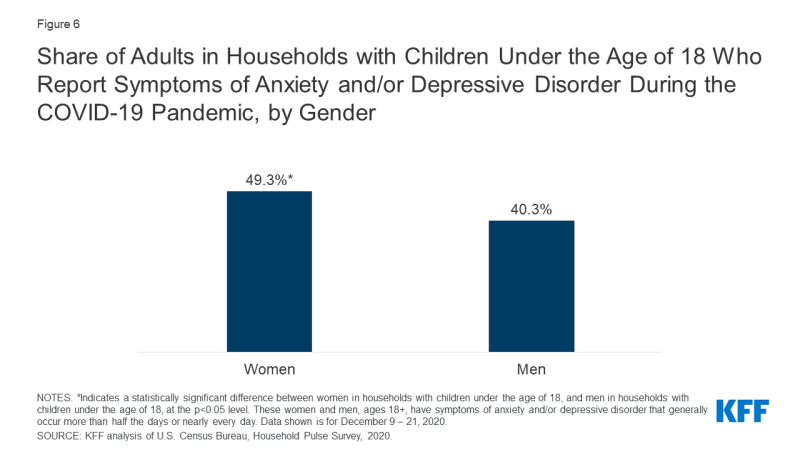
Figure 6: Share of Adults in Households with Children Under the Age of 18 Who Report Symptoms of Anxiety and/or Depressive Disorder During the COVID-19 Pandemic, by Gender
Throughout the pandemic, women have been more likely to report poor mental health compared to men. For example, 47% of women reported symptoms of anxiety and/or depressive disorder compared to 38% of men in December 2020. Among women in the workplace, more than one in four are considering leaving their jobs or reducing their hours, with many citing burnout and household responsibilities as the primary reason. Even before the pandemic, women were more likely than men to report mental health disorders, including serious mental illness.
Existing mental illness among adolescents may be exacerbated by the pandemic, and with many school closures, they do not have the same access to key mental health services. Prior to the pandemic, more than one in ten (16%) adolescents ages 12 to 17 had anxiety and/or depression.7 Children may experience mental distress during the pandemic due to disruption in routines, loss of social contact, or stress in the household. Additionally, child abuse may be increasing during the pandemic. Child abuse-related emergency department (ED) visits dropped during the COVID-19 outbreak; however, the severity of injuries among child abuse-related ED visits has increased and resulted in more hospitalizations. Child abuse can lead to immediate emotional and psychological problems and is also an adverse childhood experience (ACE) linked to possible mental illness and substance misuse later in life. Educators play a critical role in the identification and reporting of child abuse. However, with school closures and stay-at-home orders, it is likely that many cases are going undetected, and that at-risk children have increased exposure at home to their abusers.
Substance use is also a concern among adolescents. Prior to the pandemic, 15% of high school students reported using an illicit drug, and 14% reported misusing prescription opioids. Solitary substance use (as opposed to social use) has increased among adolescents during the pandemic, which is associated with poorer mental health. Suicidal ideation is yet another major concern for adolescents during the pandemic. While suicide was the tenth leading cause of deaths overall in the U.S. before the pandemic, it was the second leading cause of deaths among adolescents ages 12 to 17.8 Prior to the pandemic, suicide rates were particularly pronounced among Black and LGBTQ youth.
Communities of Color
The pandemic's mental health impact has been pronounced among the communities of color also experiencing disproportionately high rates of COVID-19 cases and deaths. Black and Hispanic adults have been more likely than White adults to report symptoms of anxiety and/or depressive disorder during the pandemic (Figure 7). This disparate mental health impact comes in addition to Black and Hispanic communities experiencing disproportionately high rates of coronavirus cases and deaths (overall as well as among health care workers and in nursing homes), and negative financial impacts. Additionally, Black parents more often than White parents have reported negative impacts of the pandemic on their children's education, their ability to care for their children, and their relationships with family members. Prior to the pandemic, Black and Hispanic people were less likely to receive needed behavioral health services compared to the general population. Additionally, deaths by suicide – which may increase due to the pandemic – have historically been much higher than average among Native American communities.
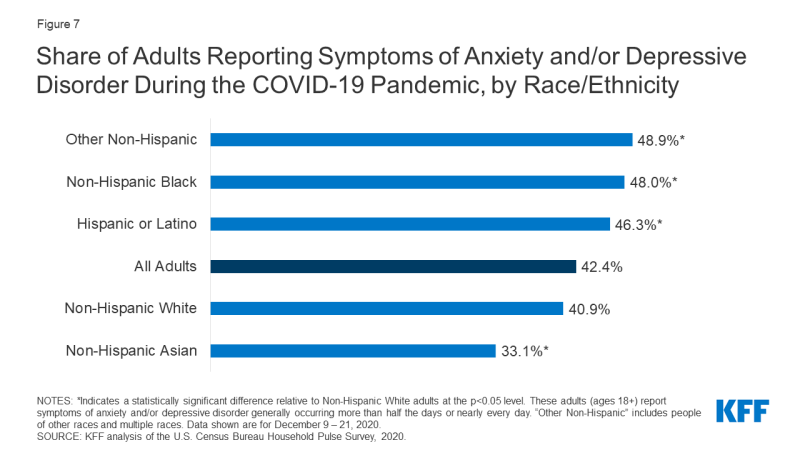
Figure 7: Share of Adults Reporting Symptoms of Anxiety and/or Depressive Disorder During the COVID-19 Pandemic, by Race/Ethnicity
Essential Workers
Essential workers during the COVID-19 pandemic, such as health care providers, grocery store employees, and mail and package delivery personnel, have shown high rates of poor mental health outcomes. These workers are generally required to work outside of their home and may be unable to practice social distancing. Consequently, they are at increased risk of contracting coronavirus and exposing other members of their household. A KFF analysis found that essential workers face additional challenges, including difficulties affording basic necessities as a result of the pandemic. These factors may contribute to poor mental health outcomes for these workers. As shown in Figure 8, essential workers are more likely than nonessential workers to report symptoms of anxiety or depressive disorder (42% vs. 30%, respectively), starting or increasing substance use (25% vs. 11%), or considering suicide in the past 30 days (22% vs. 8%).
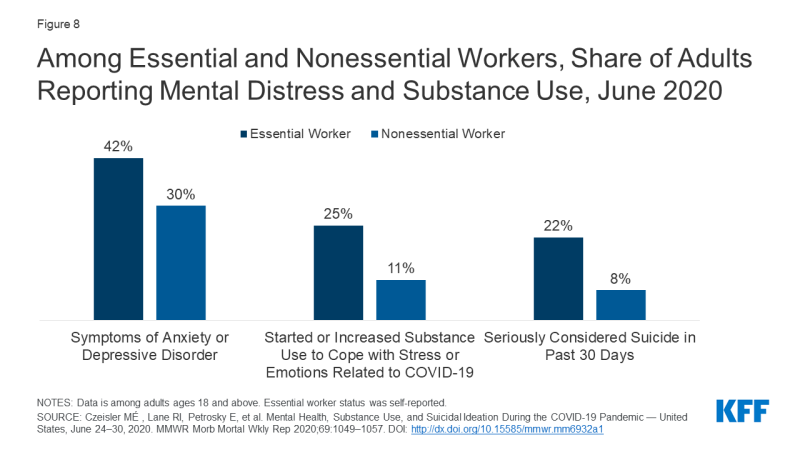
Figure 8: Among Essential and Nonessential Workers, Share of Adults Reporting Mental Distress and Substance Use, June 2020
During the pandemic, frontline health care workers have reported feelings of anxiety and depression and thoughts of suicide. The KFF Health Tracking Poll conducted in mid-April 2020 found that 64% of households with a health care worker said worry and stress over the coronavirus caused them to experience at least one adverse impact on their mental health and well-being, such as difficulty sleeping or eating, increases in alcohol consumption or substance use, and worsening chronic conditions, compared to 56% of all households. Prior to the pandemic, nurses and physicians were already prone to experiencing burnout, with physicians also having an elevated risk of suicide.
Policy Responses and Considerations
Throughout the pandemic, leading public health organizations — including the CDC, SAMHSA, the World Health Organization, and the United Nations — have released general considerations and resources addressing the mental health and well-being of both general populations and specific, high-risk groups during the pandemic. In the U.S., some steps have been taken at both the federal and state levels to address the pandemic's impact on mental health, but with mental health problems on the rise, key issues are likely to persist.
Congress has addressed some of the acute need for mental health and substance use services through two stimulus bills enacted during the pandemic. The Consolidated Appropriations Act, which was signed into law in December 2020, includes about $4.25 billion in funding for mental health and substance use services. It also builds on existing legislative efforts to boost insurer compliance with federal mental health parity rules. The Coronavirus Aid, Relief, and Economic Security Act (CARES Act), a stimulus bill passed in March 2020, also allocated funding for mental health and substance use services, including a $425 million appropriation for use by SAMHSA, in addition to several provisions aimed at expanding coverage for, and availability of, telehealth and other remote care for those covered by Medicare, private insurance, and other federally-funded programs. It also allowed for the Department of Veterans Affairs to arrange expansion of mental health services to isolated veterans via telehealth or other remote care services. Other efforts to address mental health needs include substantial increases in the use of telehealth for mental health services, aided early on by the federal government and many states expanding coverage and relaxing regulations for telehealth services. Looking ahead, the Biden administration and Congress could take additional steps to address mental health and substance use issues, including administrative actions addressing suicide among LGBTQ youth, mental health parity, the opioid crisis, veteran mental health services, and school-based mental health services.
Given the pandemic's implications for both people with new or pre-pandemic mental health conditions, the crisis spotlights new and existing barriers to accessing mental health and substance use disorder services. Among adults reporting symptoms of anxiety and/or depressive disorder, more than 20% report needing but not receiving counseling or therapy in the past month during the pandemic. Limited access to mental health care and substance use treatment is in part due to a current shortage of mental health professionals, which has been exacerbated by the pandemic. The pre-pandemic shortage of psychiatric hospital beds has also worsened with the surge of COVID-19 patients needing beds at hospitals across the nation.
Access to mental health and substance use care was a concern prior to the pandemic. In 2018, among the 6.5 million nonelderly adults experiencing serious psychological distress, 44% reported seeing a mental health professional in the past year. Compared to adults without serious psychological distress, adults with serious psychological distress were more likely to be uninsured (20% vs 13%) and be unable to afford mental health care or counseling (21% vs 3%).9 For people with insurance coverage, an increasingly common barrier to accessing mental health care is a lack of in-network options for mental health and substance use care. Those who are uninsured already face paying full price for these and other health services. As unemployment continues to affect millions of people, who in turn may lose job-based coverage, some may regain coverage through options such as Medicaid, COBRA, or the ACA Marketplace, but others may remain uninsured. With an unprecedented share of people reporting symptoms of anxiety or depressive disorder, the potential outcome of California v. Texas (a case challenging the constitutionality of the entire ACA) is important to consider. Prior to the ACA, people with a preexisting condition like depression might have been denied health coverage or charged higher premiums, and many individual market plans did not cover any mental health or substance use services.
Looking Ahead
The pandemic has both short- and long-term implications for mental health and substance use, particularly for groups at risk of new or exacerbated mental health disorders and those facing barriers to accessing care. Phased COVID-19 vaccinations are taking place across the country, perhaps signaling that the end of the pandemic is on the horizon. However, many of the stressful conditions employed to mitigate the spread of the coronavirus are likely to persist for the near future, given the slow and troubled rollout of vaccinations across the country, instances of people refusing the vaccine due to fear or uncertainty, and the need for vaccinated people to continue taking existing precautions to mitigate the outbreak.
History has shown that the mental health impact of disasters outlasts the physical impact, suggesting today's elevated mental health need will continue well beyond the coronavirus outbreak itself. For example, an analysis of the psychological toll on health care providers during outbreaks found that psychological distress can last up to three years after an outbreak. Due to the financial crisis accompanying the pandemic, there are also significant implications for mortality due to "deaths of despair." A May 2020 analysis projects that, based on the economic downturn and social isolation, additional deaths due to suicide and alcohol or drug misuse may occur by 2029.
As policymakers continue to discuss further actions to alleviate the burdens of the COVID-19 pandemic, it will be important to consider how the increased need for mental health and substance use services will likely persist long term, even if new cases and deaths due to the novel coronavirus subside.
This work was supported in part by Well Being Trust. We value our funders. KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities.
How to Get Your Gun Rights Back for Mental Illness
Source: https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/
0 Response to "How to Get Your Gun Rights Back for Mental Illness"
Post a Comment